the good doctor on: COVID-19 & Dry Eye

Blog #32
We are almost there.
As we get news of Britain’s immanent unrolling of Pfizer’s COVID-19 vaccine, we have reason to be hopeful. We, here in Canada, are likely 3 to 4 months away from our own full-scale program. We must hang on. The mask is still our best defense against the virus.
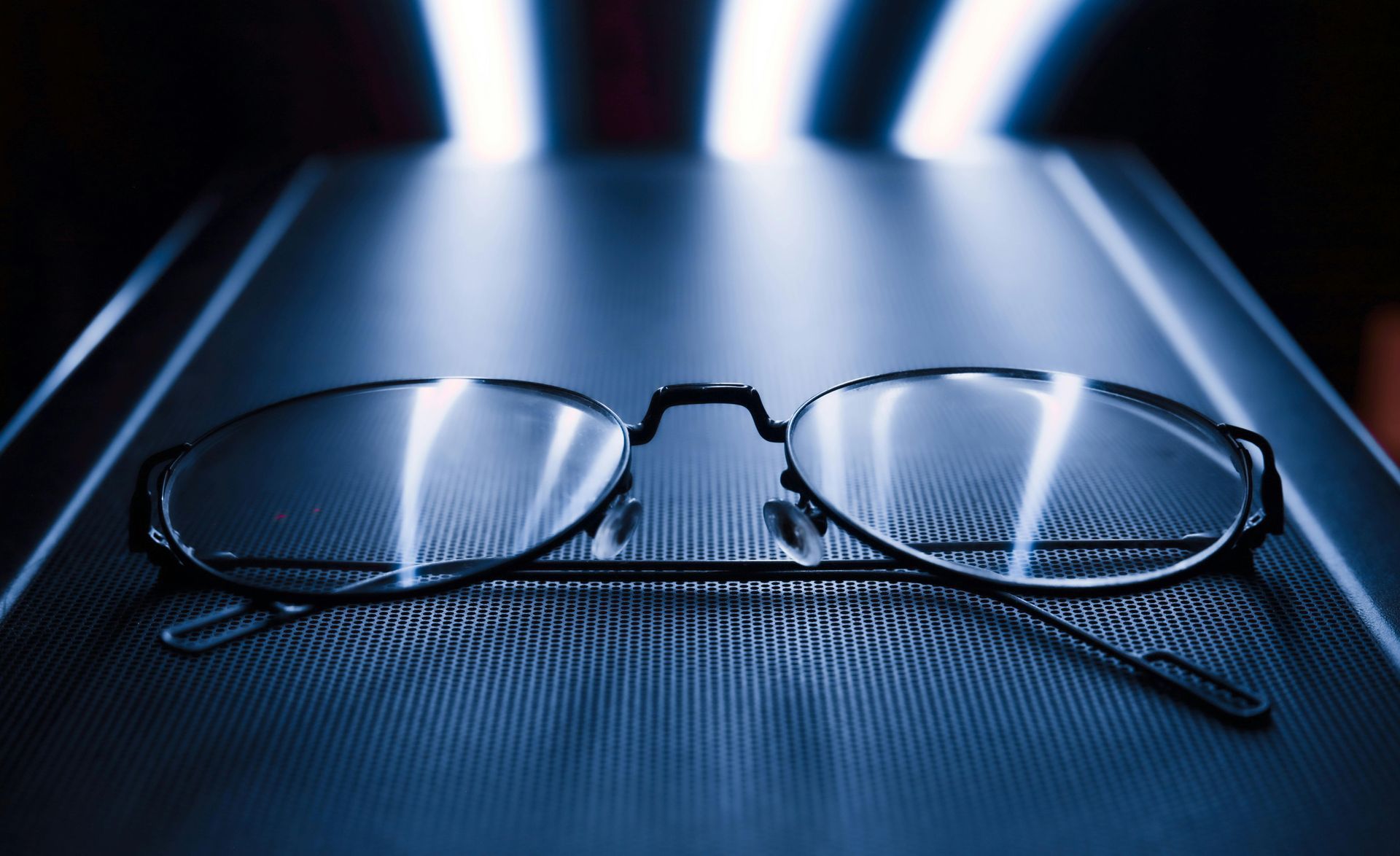
A recent article in the journal Eye , addressed a COVID-related problem. The wearing of masks can create surprising complications with the eyes in some situations. In the article, a patient recovering from cataract surgery presented after a few hours with substantially reduced vision. Upon examination, the clinic found that the patient was experiencing symptoms of extreme dryness from the wearing of an ill-fitting mask. When there are openings in the top of the mask, the airflow gets redirected over the vulnerable ocular surface. In this case the combination of an anesthetized eye that could not react to drying, and the reversed airflow, left the cornea too exposed. The clinic was able to relieve the patient and recovery progressed in a healthy manner.
Extreme dry eye has also been noted in patients using ventilators in ICU or in people wearing a CPAP for obstructive sleep apnea. If drying persists, the cornea can be damaged and the risk of infection greatly increases, especially when exposed to the droplets that come from the patient’s own breath, ironically.
Make sure that your mask fits well and does not redirect air over your eyes. At Burlington Eyecare we have been using surgical tape over the top of patient’s masks to help reduce this airflow (it helps to keep our equipment from getting fogged up). The key here is to have a well fitted mask. Remember that eye dryness is a potential problem that can easily be treated or avoided, but can have surprisingly serious consequences if left unchecked.
Til next week,
The Good Doctor, Dr. Mark Germain, Burlington Optometrist