Ocular Conditions
Age-Related Macular Degeneration (AMD)
What Is It?
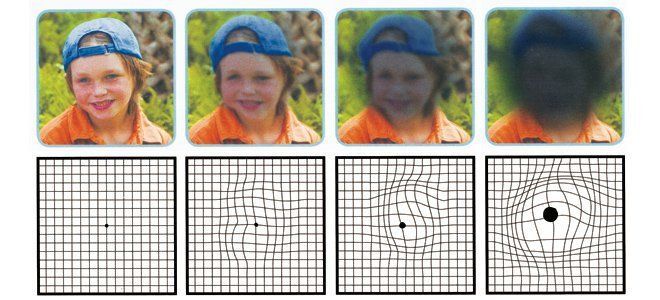
The macula is a small yet very important area of the retina. It is responsible for providing us with our central, fine-detailed 20/20 vision. Age-Related Macular degeneration (also referred to as AMD) is the number one cause of vision loss in the western world. AMD is typically associated with central vision loss.
There are two forms of Macular Degeneration. The most common form, accounting for approximately 90% of all cases, is referred to as “dry” because no fluid is involved. Unfortunately, it can progress to the “wet” form, where leakage of fluid inside the eye causes swelling and scarring.
How Do We Diagnose It?
In early stages, AMD is symptom free but can be diagnosed in a routine Comprehensive Eye Exam. Initially, patients will typically report blurred central vision while trying to see fine detail. Glasses or contact lenses are unable to correct this and over time the area may become larger interfering with reading and recognizing faces. AMD can also cause distortion making straight lines appear wavy and dark spots can obscure parts of the central vision. There is no pain associated with AMD. When AMD is present, we take digital fundus photographs of the macula to monitor. The OCT (Optical Coherence Tomographer) also aids in detecting more subtle changes. These tests will also tell us if/when wet AMD is starting.
How Do We Treat It?
Most treatments for “dry” AMD are lifestyle changes such as exercise, discontinuing smoking, wearing sunglasses to reduce UV radiation and Vitamin Supplements made specifically for ocular health.
Cases of wet AMD can be treated with a medication which is injected into the eye in an attempt to stop blood vessels from leaking and also to reduce the eyes ability to build new blood vessels (which can result in more leakage and scarring).
It is extremely important to intervene with wet AMD as soon as possible in order to retain vision. Regular eye examinations and counselling from your Doctor of Optometry will let you know when new treatments become available.
Can It Be Prevented?
As is the case with most Eye Diseases, UV protection and nutrition are critical for prevention. Lack of UV protection and poor nutrition result in free radicals which damage receptor function. Again, cigarette smoking is very harmful. A balanced diet with emphasis on antioxidants such as lutein can help to prevent or stop the progression of, and in some instances mildly reverse the condition. Ocular vitamins can also help stop or reduce further degeneration.
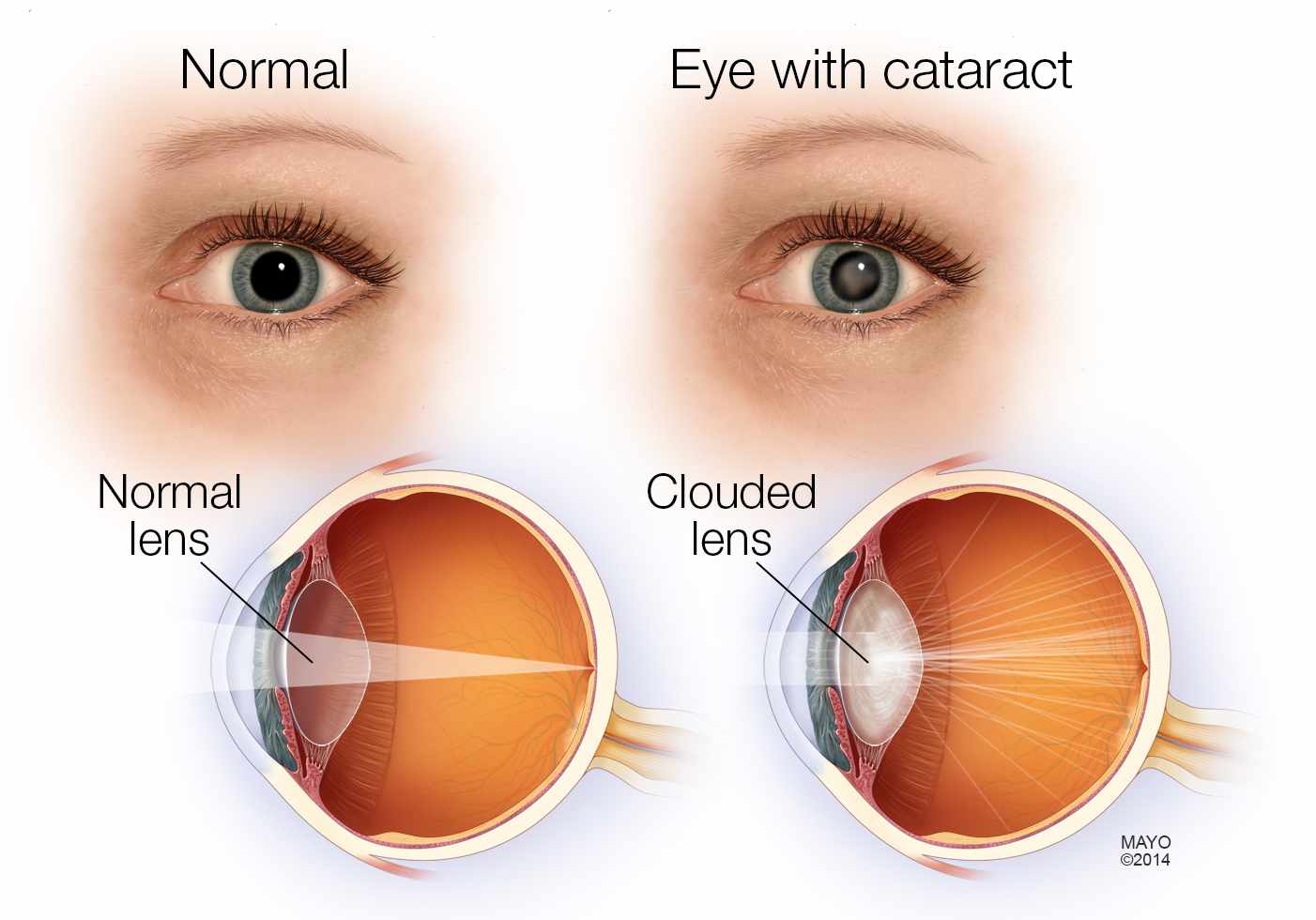
Cataracts
What Is Cataracts?The crystalline lens is located in the eye near the front and remains clear for most of our younger days, but in time can become cloudy resulting in hazy vision and glare problems known as a cataract. Exposure to ultraviolet light and other forms of radiation, nutrition deficiencies, certain medications, aging and severe head trauma are known to be causes. In rare cases children can be born with cataracts, commonly referred to as Congenital Cataracts.
How Do We Diagnose Cataracts?
Our optometrists can spot a cataract forming at the very beginning stages through a comprehensive eye exam. Using the slit lamp the doctor is able to asses the clarity of the lens and determine if there is any opacity indicating a cataract.
How Do We Treat Cataracts?
When cataracts become troublesome, they can be removed and replaced by an implant through micro-surgery. In some cases haze may develop after cataract surgery, and a quick laser procedure with an ophthalmologist can remove this. Patients should return to their optometrist 4-6 weeks following their procedure for post operative care and vision evaluation.
Can Cataracts Be Prevented?
A balanced diet, UV protection and choosing not to smoke will certainly help to slow the process. It is important to ensure that you are always wearing 100% UV protection sun wear whenever the sun is out in all types of weather to protect your eyes.
Diabetes & Diabetic Retinopathy
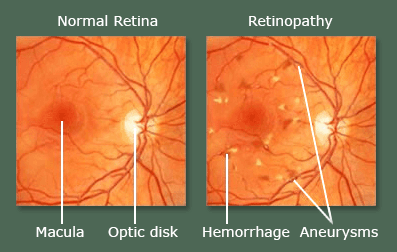
What Is Diabetic Retinopathy?Diabetes is a chronic, often debilitating and sometimes fatal disease, in which the body either cannot produce insulin or cannot properly use the insulin it produces. Diabetes leads to high blood sugar levels, which can damage organs, blood vessels and nerves. If there is a blood vessel leak, it can leak into the retinal layers of the eye which, if not treated, can result in severe and permanent vision loss from scarring (Referred to as Diabetic Retinopathy). When sugars are not under control, it can also cause fluctuations in vision and/or cataracts.
How Do We Diagnose Diabetic Retinopathy?
Those who have diabetes will typically be diagnosed by their family doctor. These patients are covered by OHIP regardless of age for a full annual eye exam. During these comprehensive eye exams, our optometrist will dilate and look into the eye using a Slit Lamp to look for signs of diabetes affecting the inside of the eye.
At Burlington Eyecare we use a sophisticated 3-D imaging device called an OCT (Optical Coherence Tomography) which will allow the Optometrists to view the Fundus and Macula to ensure no damage has been caused by the symptoms of diabetes and to monitor conditions annually.
How Do We Treat Diabetic Retinopathy?
Treatment for Diabetic Retinopathy is provided by an ophthalmologist using laser treatments, injections, or a combination of both, depending on the severity and location of the leakage.
Can Diabetic Retinopathy Be Prevented?
Currently in Canada 90% of patients living with diabetes have Type II Diabetes with the main causes attributed to obesity and a sedentary lifestyle. Living an active and healthy lifestyle can reduce the risk and even alleviate it.
Some people inherit diabetes, and in spite of preventative measures, have difficulty controlling it. Medication helps to improve glucose uptake and regular monitoring of the blood for glucose levels and glycosylated hemoglobin aid in keeping the diabetes under control. Daily regulation of sugar, calorie intake and metabolism help to control blood sugar levels. The importance of an annual physical examination by your family doctor, as well as an annual eye health examination by your optometrist are not to be underestimated.
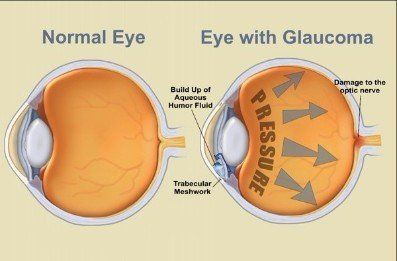
Glaucoma
What Is Glaucoma?Glaucoma is a group of progressive eye diseases which damage the eye's optic nerve and can lead to permanent damage and vision loss.
How Do We Diagnose Glaucoma?
At Burlington Eyecare, our pre-testing procedures include various pre-screening tests for Glaucoma such as a Visual Fields Test as well as NCT (Non-Contact Tonometry). If during this pre-screening there are any indications of high pressure or peripheral vision loss, our optometrist will request futher diagnostic tests. These can include a more detailed visual field test, further eye pressure monitoring, as well as an OCT (Optical Coherence Test).
How Do We Treat Glaucoma?
Treating Glaucoma depends on the level of severity and progression. In most cases treatment includes eye drops prescribed to reduce the intraocular pressure (IOP). Although there is no known cure, these drops help to control the IOP to prevent further damage. In some instances when the drops cannot control the pressure, various surgical options may be used to further increase fluid outflow, thereby lowering the eye pressures further. Any vision that is lost due to Glaucoma cannot be repaired, which is why regular comprehensive exams from an optometrist are integral to eye health.
Can Glaucoma Be Prevented?
In some families, Glaucoma can have a hereditary link, therefore a knowledge of your family's current ocular history is important. Those with diabetes, high blood pressure or a history of injury to the eye have a higher risk of developing Glaucoma. Glaucoma cannot be detected without a comprehensive eye exam. It is often symptomless.
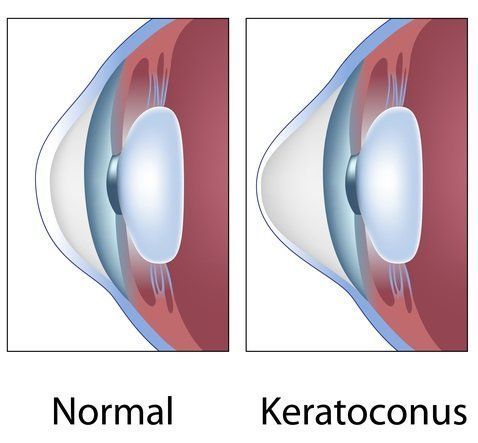
Keratoconus
What Is Keratoconus?Keratoconus is a corneal disease that occurs when the normally round dome-shaped cornea (the clear outer area of the eye) progressively thins, causing a cone-like bulge to develop. It is typically diagnosed during adolescence and early adulthood with a variable rate of progression. Since the cornea is responsible for refracting most of the light coming into your eye, an abnormally-shaped cornea can create reduced visual acuity and affect the way you see. This reduced visual acuity can make even simple daily tasks, such as driving, watching television or reading, difficult to perform, even while wearing glasses or contacts.
How Do We Diagnose Keratoconus?
Various indicators can be noted using slit lamp examination and corneal topography (a map of the shape of the cornea).
How Do We Treat Keratoconus?
Keratoconus cannot be cured, but there are several methods for managing Keratoconus to help slow its progression and help improve vision. Hard contact lenses are often used to give the eye a new smooth surface which helps refract the light in a more uniform manner. This provides much clearer vision.
There are also various treatments including Intra-Corneal Ring Segments (INTACs) which can surgically alter the corneal surface to minimize the severity of central steepening. Corneal Crosslinking is a newer treatment that uses Riboflavin and UV light to strengthen the collagen fibers of the cornea. This helps to slow or even stop the progression of corneal bulging, and when treated early enough, will make future correction with glasses or contact lens wear more successful. At Burlington Eyecare, we co-manage your treatment with TLC to provide this therapy. In more severe cases, patients may require a corneal transplant.
Can Keratoconus Be Prevented?
Keratoconus is very difficult to prevent. It can be hereditary and has shown some link to excessive eye rubbing and those with Down Syndrome.
Low Vision Impairment
What Is Low Vision?Low vision, or visual impairment, is reduced vision despite using the best-possible spectacle or contact lens correction available. It can result from congenital eye conditions, such as retinitis pigmentosa, or acquired eye conditions, such as diabetic retinopathy or macular degeneration.
How Do We Diagnose Low Vision?
In order to determine which types of aids would benefit a patient, a low vision specialist performs an assessment to establish the patient's best possible vision, baseline glasses prescription and the patient's goals and expectations. The optometrist selects aids based on the aforementioned factors and provides instruction and direction as to how to use these aids.
How Do We Treat Low Vision?
The role of a Low Vision Specialist is to maximize the functional level of a patient's vision through optical and non-optical means. This is done primarily through magnification, filters and proper lighting. For distance tasks, like recognizing faces, watching TV or reading signs, a low vision optometrist may suggest telescopes, either hand-held or mounted on the glasses. For near tasks, such as reading books or needle work, they may suggest one of many types of magnifiers.
At Burlington Eyecare, we perform assessments using only the best products available by Eschenbach. Their assortment of spectacle and clip-on magnifiers, hand-held magnifiers, stand magnifiers, telescopes, absorptive filters, video magnifiers and many non-optical tools such as lighting and reading stands, help us to meet the needs of our patients with visual impairments.
Can Low Vision Be Prevented?
The Assistive Device Program (ADP) through the Government of Ontario provides support and funding to Ontario residents who have long-term physical disabilities and provides access to personalized assistive devices appropriate for the individual's basic needs. Your optometrist can assess your low vision needs and assist in qualifying for support through ADP. Dr. Germain of Burlington Eyecare is an ADP-Registered Authorizer and he will work with patients to seek funding through ADP.
Please do not hesitate to contact Burlington Eyecare if you have any questions regarding our Low Vision Services (commonly referred to as Low VA), the Assistive Devices Program, or low vision in general.