A low vision prosthetic that actually works

Blog vol 6.16. A low vision prosthetic that actually works.
A topic that is very close to my heart and one of my biggest interests: low vision.
Over the past 35 years I have worked with many visually impaired patients. The number one condition that causes vision loss in North America is macular degeneration. Over the years we have done much to prevent and reduce the effects of the disease: reduced incidence of smoking, more balanced diets, as well as improved treatments and diagnostic tools.
There remains a group of patients that have a form of “dry” macular degeneration, called geographic atrophy, that still suffer serious vision loss. An ophthalmologist from Stanford, Dr. Daniel Palanker, wanted to change that. It was back in 2005, when working with ophthalmic lasers, that he began to dream of using light to treat visual impairment.
For some time, ophthalmologists have been experimenting with implant microchips in the back of the eye. The old implants were electrically wired to the visual system from the macula — hard to install, cumbersome, and the resulting vision not great.
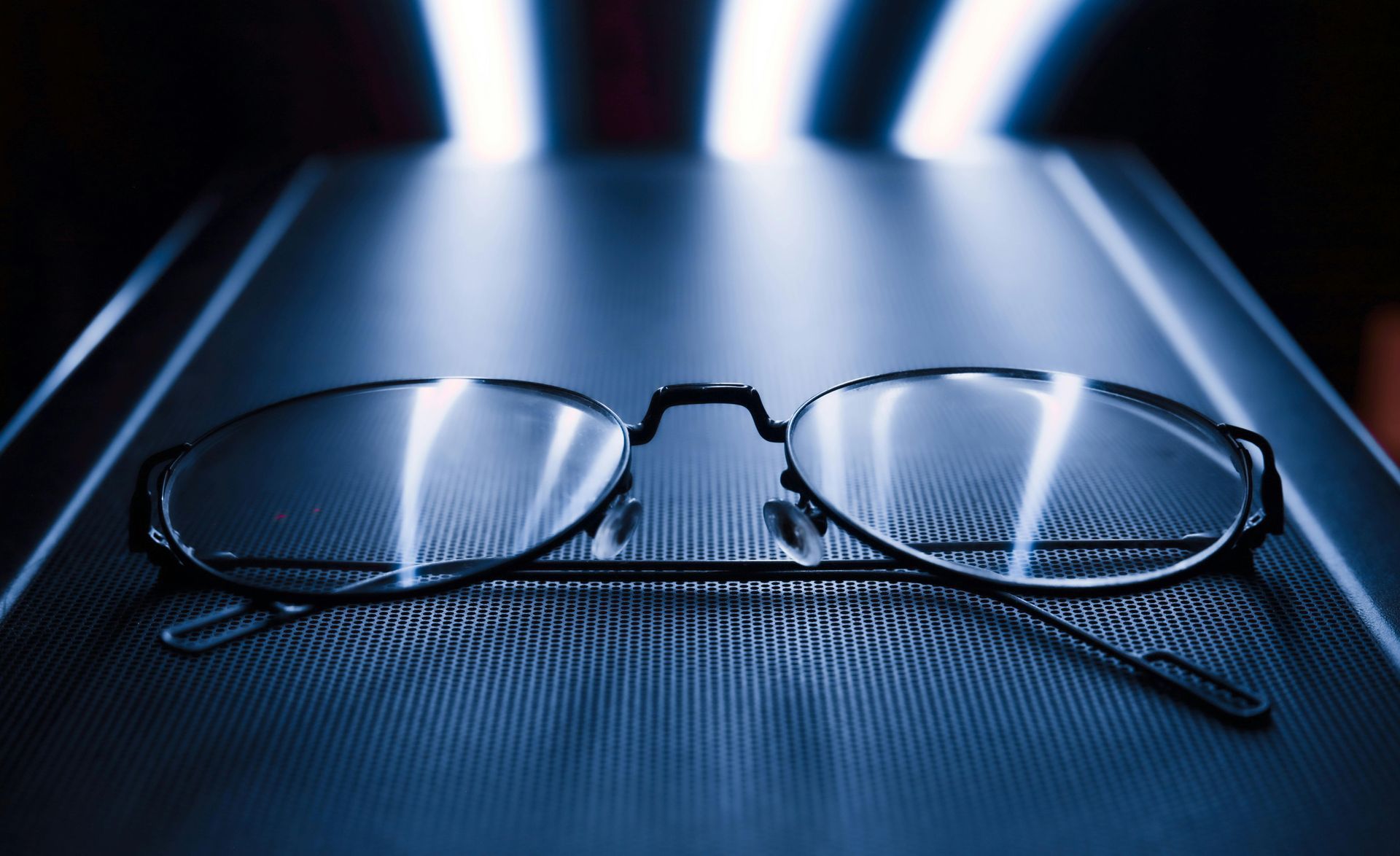
Dr. Palanker’s working hypothesis was that macular degeneration did not damage the inner retinal neurons; some diseases (like glaucoma) can destroy all layers of neurons. Consequently, he designed a retinal prosthesis that replaces the damaged outer segment’s photoreceptors. The prosthesis includes a microchip which is implanted in the back of the eye and a pair of glasses that communicates with it.
A microchip was developed that receives photons of light and converts them into electrical signals that are in turn transmitted through the retinal and visual pathways to the visual cortex. Then he developed special glasses that have a built-in camera and a near infrared transmitter that stimulates the embedded microchip at the retina (the back of the eye). The infrared does not stimulate the “healthy” peripheral retina thus reducing confusion when perceiving light.
Installing the microchip involves detaching the inner retina from the damaged outer, sliding the chip in place, then reattaching the inner retina over it. The sensor is photovoltaic, receiving its energy from the incoming infrared, so no wires. There is a considerable learning curve when adapting to the device and the camera on the glasses comes with controls for brightness, contrast, and magnification.
The current prototype uses a black-and-white image, but there are already improvements being made. Software is being developed to create gray-scaled images which help with things like facial recognition. The present microchip has pixels that are 100 microns wide, with 378 pixels per chip. The next generation chip will have pixels that are 20 microns wide, with 10,000 pixels per chip. This new chip will have the potential to get to 20/80 vision and even down to 20/20 with “electronic zoom”. Read some of the latest research at Stanford here.
What a great idea! The years of refining and improving retinal prosthetics is paying off. Time to line up some of my patients that could really benefit from this new technology.
‘til next week,
The good doctor