the good doctor on: Last Week: Spurge, ThePlant; This Week: Stems…

Blog.Vol.II.23 Last Week: Spurge, The Plant; This Week: Stems…
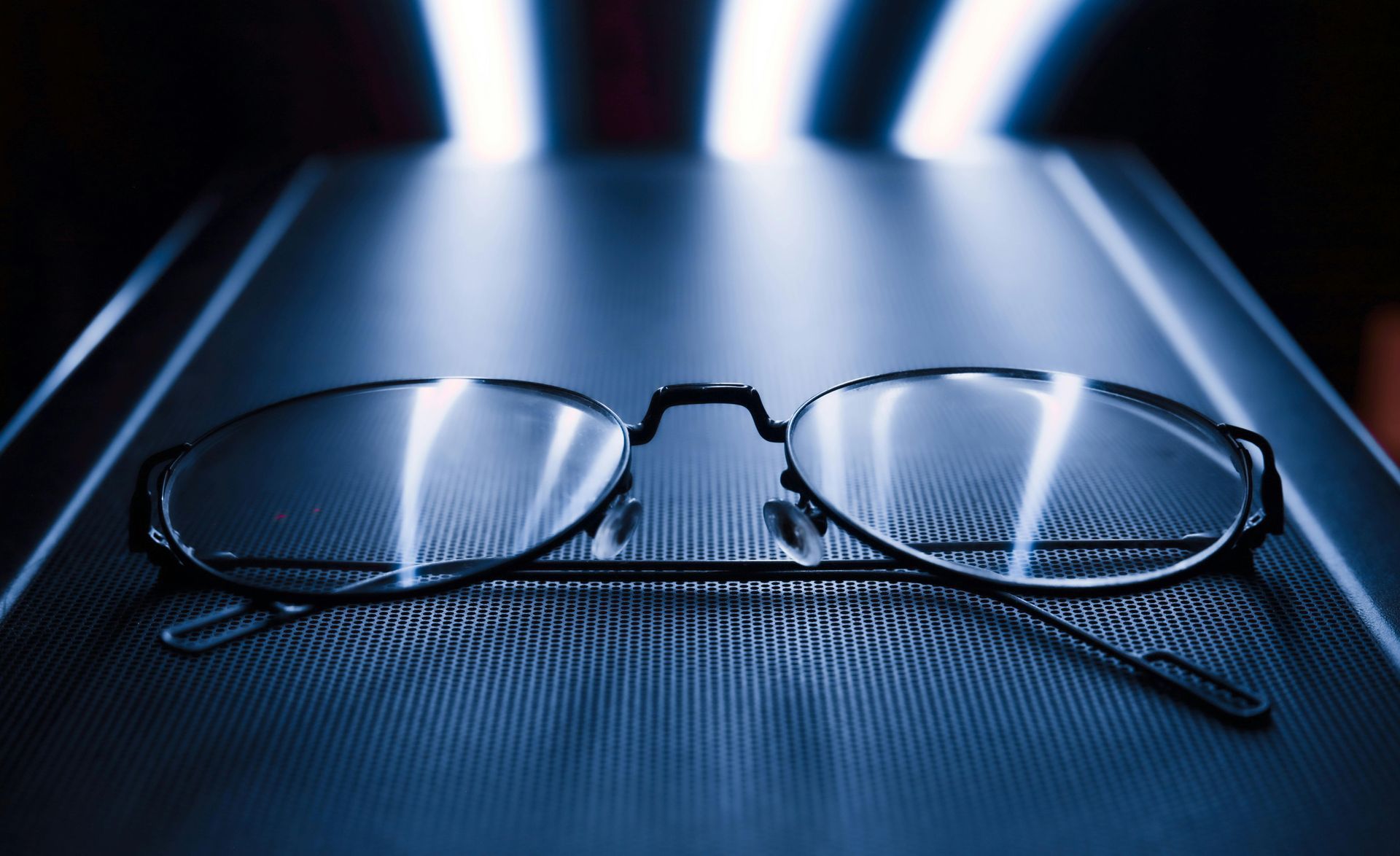
… actually, stem cells. I receive a weekly news feed from the journal, Nature, that keeps me informed on the latest research, especially when it comes to eyes. This week featured regenerative therapy in which researchers are using stem cells to “regrow” vital tissues in the eye. The most recent research has been in replacing damaged corneal epithelial cells, photoreceptors like cones, retinal pigment cells, and ganglion cells, different parts of the eye.
Stem cells have been the source of much research in the past few decades. They are body cells that have not differentiated into specific tissues. The research related to the eye has been with a class of cells called induced pluripotent stem cells, or iPS cells, which are harvested from the donor, coaxed into becoming stem cells, then into more specific tissues like retinal epithelial cells. The researchers harvest these cells from the donor’s own tissue which makes rejection of the newly grown tissue unlikely, a huge advantage.
When the cornea is severely damaged by a chemical burn, intense UV burn, or an explosive, it must be replaced. The donor cornea replaces the central 8 mm of cornea in these cases. The corneal epithelium regenerates from stem cells that are at the limbal area, just next to the cornea. But if damage is extensive, then these cells cannot be produced and migrate to replace old corneal cells. The unfortunate result is a short-lived transplant. With stem cells obtained from a healthier limbus and cultured, these stem cells can be implanted into the damaged eye and help sustain the transplant.
A similar procedure is used when restoring the retina. Researchers are finding ways to coax stem cells into more specialized tissues like retinal pigment epithelium and photoreceptors, which are damaged in macular degeneration, diabetes, or retinitis pigmentosa. Stem cells are also being used to develop new ganglion cells, which are damaged in glaucoma. In the past, stems cell were injected into the affected retina, in the hope that they would organize into functional tissue. This strategy was not very successful, with more promising results from the production of “sheets" of stem cells that are then mounted into the retina. Much work still needs to be done, but this is very hopeful.
These are exciting times. All of this means that there are possible treatments for previously devastating eye conditions hopefully just around the corner.
Keeping you posted, til next week,
the good doctor, Dr. Mark Germain, Burlington Optometrist