Nice to be back
Blog vol 3. 27 Nice to be back.
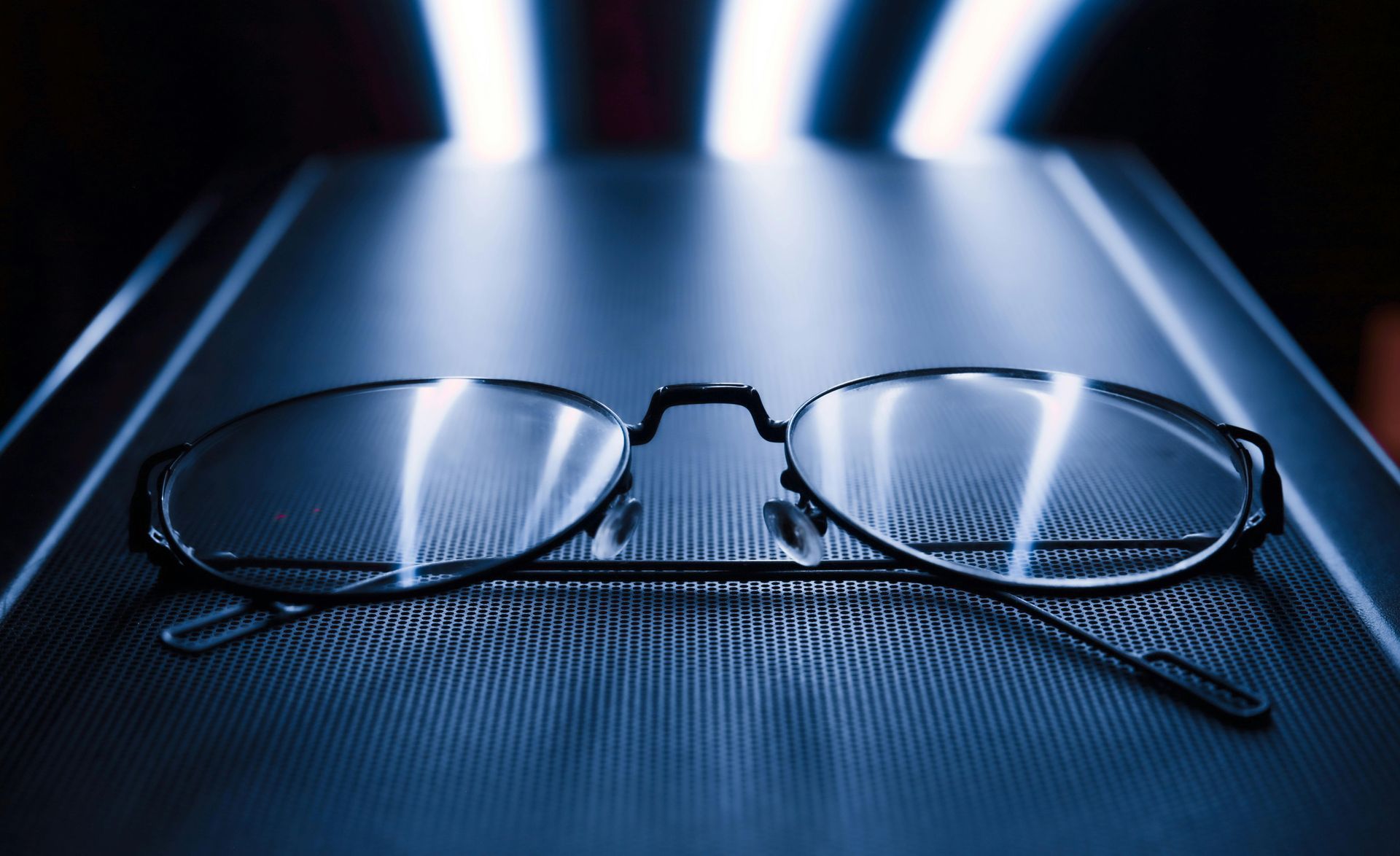
Last week we looked at the post covid resumption of Medical Ministry International (MMI) eye missions. Another new post-covid experience, this past weekend I had the pleasure of meeting up with my colleagues at a continuing education event hosted by the Waterloo School of Optometry. Really nice to meet up with old friends and learn what is new in eye care.
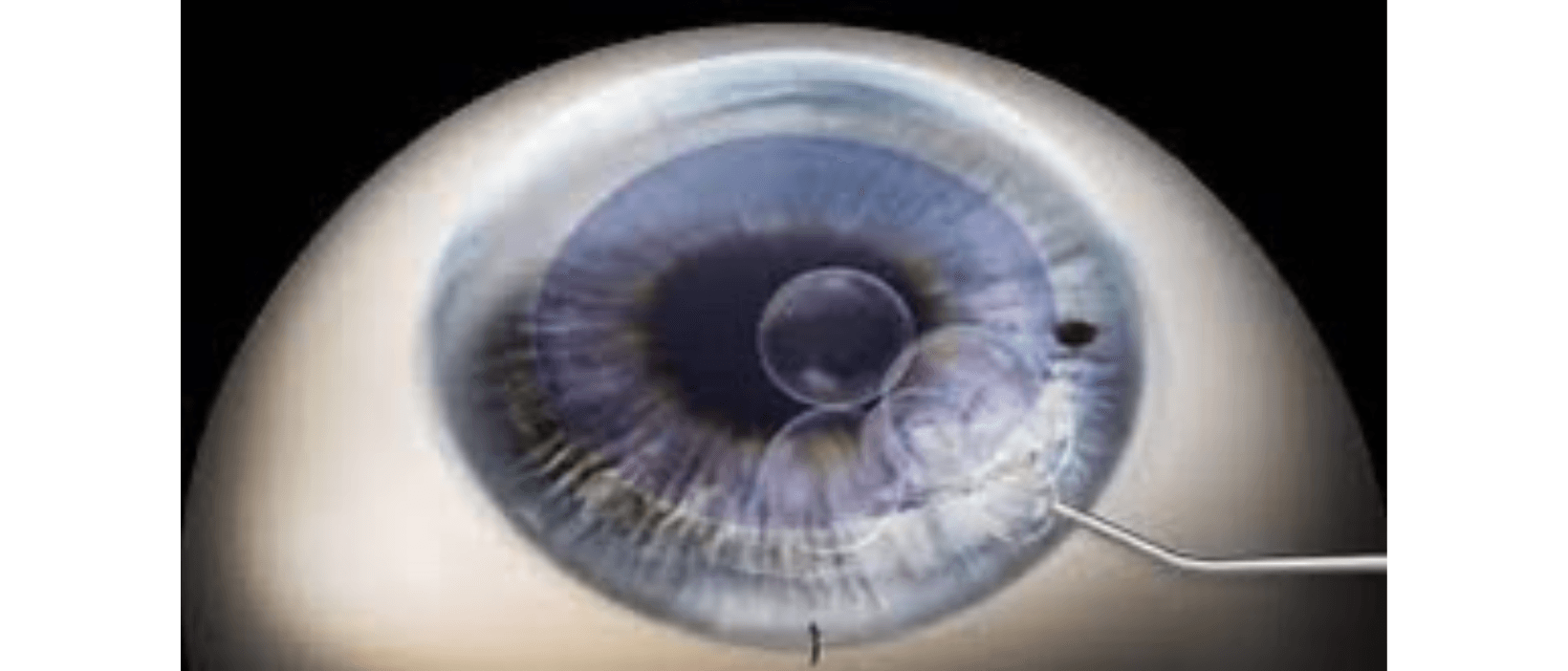
A local eye surgeon made a presentation on procedures around routine cataract surgeries. The procedure I was most interested in was Descemet Membrane Endothelial Keratoplasty (DMEK). That is a mouthful. This procedure is done when the back layer of the patient’s cornea, the endothelium, has broken down and the surgeon replaces it with a very thin layer of donor cornea.
The DMEK procedure was first successfully done in 2006. Before this, the only way to replace the layer, the corneal endothelium, was to remove the whole cornea and replace it with a whole new donor cornea, very involved, with a large risk of graft rejection and reduced visual outcomes.
The key to the DMEK is the donor tissue preparation, being able to dissect a 10-15 micron thick layer of the cornea from the donor. This kind of precision was just not possible in the past. The surgeon jokingly lamented that they were getting such great results that patient expectations had also risen leaving less room for difficulties.
Now, patients being assessed for cataract surgery get their corneal endothelium measured for integrity as a matter of routine. This is a recent development and a good one. In the past (a year or so ago), the need for a transplant cornea wasn’t discovered until post-cataract surgery when the patient found they were not recovering their vision as they should. Then the patient needed to be reassessed and a separate surgery scheduled, with much more wear and tear on everyone.
Now, if the initial assessment shows that the patient requires the DMEK procedure, it is done right away during the cataract surgery. They call it a triple DMEK. Several of my cataract patients have required DMEK and had good results. For more details on DMEK click here.
This is a wonderful procedure, making clear vision possible for people who would no longer have it, but as with any transplant, the patient needs a steroid drop indefinitely to reduce the possibility of graft rejection. Rejection is a possibility.
When I started to practise in 1987, the only option for these patients was a full corneal graft; this newer procedure is a vast improvement with a lot shorter recovery time and great visual results.
Thank you to the eye surgeons who hone their skills and provide wonderful eye care.
til next week,
the good doctor